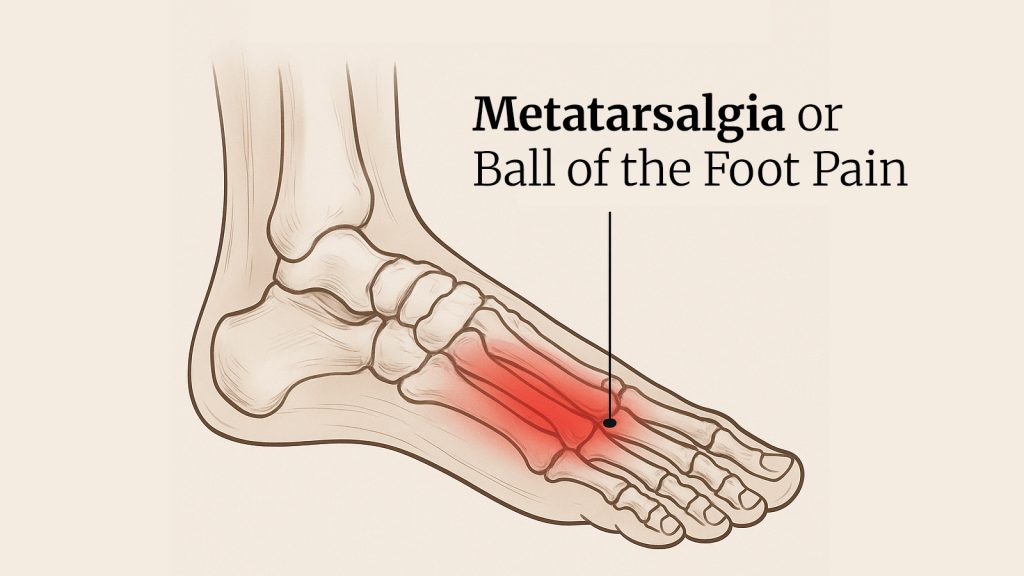
What is Metatarsalgia?
Metatarsalgia, also referred to as ball-of-the-foot pain, is a disorder of the forefoot that implies pain and inflammation. The individuals usually refer to the feeling as walking on pebbles or having a bruise under the ball of the foot. This kind of pain is generally localized underneath one or several heads of metatarsals, which are the five long bones linking the feet in the mid-foot and the toes. Most symptoms become more aggravated when standing up, walking, or running, as well as having redness on the skin of the foot, callus buildup, and pain on toe flexing. Primary care includes self-treatment with rest, ice, and conversion to low-impact exercises to minimize pressure and inflammation.
Metatarsalgia is not a single condition; it is symptomatic of other conditions, which are usually broken down into three groups.
Primary Metatarsalgia: This occurs when there is a structural issue with the foot that results in pain under one or more metatarsal heads, which causes the front portion of your foot to experience uneven pressure distribution. Bunions or hammertoes, a high arch (pes cavus), or a longer second toe can all shift an excessive amount of weight onto certain metatarsal heads; this can result in pain and inflammation.
Secondary Metatarsalgia: This type often results from outside or internal factors contributing to an overburden of the forefoot. The standard drivers are obesity, pregnancy, secondary arthritic conditions like rheumatoid arthritis, diabetes, and the use of unsupportive footwear. For successful treatment, it is essential to manage the source of the problem.
Iatrogenic Metatarsalgia: This can develop as post-traumatic or as a consequence of prior foot surgery. Some surgeons worry that realignment of the bones in the foot -especially those in the big toe- may transfer pressure to other metatarsal heads, causing a new source of discomfort. Typically, a callus develops in this area. When postsurgical pain indicates a pressure transfer, we have to consider a reevaluation of the alignment of the foot.
How Common Is Metatarsalgia?
Metatarsalgia is very common and affects both non-athletes and athletes, but is more likely in runners and high-impact athletes, where increased stress on the underfoot occurs every time the foot hits the ground -such as jumping, sprinting, etc. People wearing the wrong shoes and walking barefoot on the forefoot for an extended period or having foot deformities like bunions are predisposed to it, and so are overweight people or pregnant women. Another significant risk is the frequent use of high heels.
What are the Symptoms of Metatarsalgia?
Metatarsalgia can cause a burning or sharp pain in one of the balls of your foot, while for some, it feels like there’s a rock in their shoe. This may include the formation of huge calluses under the heads of metatarsals, which are painful. And sometimes, other people feel a “tingly” or “numb” feeling in their toes. It usually gradually worsens over several months, and the pain gets worse as patients walk or run.
What Causes Metatarsalgia?
Metatarsalgia is caused by a disruption in the balance of weight that propagates across one or more of the five long metatarsal bones in your midfoot, also known as the forefoot. This pressure is generally due to the constant movement that one gets through activities like running, jumping, and walking. The kind of shoes you wear may also play an important part; shoes with skinny soles, a good match, or excessive heels force extra weight and tension into the forefoot. Some anatomical factors play a role, too. For example, if you have a foot with normal metatarsals but a short first metatarsal bone or hypermobility of your first ray, it will change your weight distribution. It can cause overloading of the rest of your metatarsals, increasing the chance of getting metatarsalgia. Such pressure can manifest in several ways, including:
- Foot deformities: A deformity, such as hammertoes or claw toes, causes the joints to be in a distorted location, thus causing unequal distribution of the weight. When they occur, a bunion (hallux valgus) can redistribute weight-bearing off the first metatarsal and onto the lesser metatarsals. Moreover, there is an elevated arch (pes cavus), which elevates the insole pressure to the forefoot and the rear of the heel.
- Improper footwear: Footwear with thin soles, narrow toe boxes, or heels puts undue strain on the ball of the foot. In particular, in high heels, considerably more of the body weight is placed on the metatarsal heads. Mismatched shoes may even aggravate the presence of deformities in the feet.
- High-impact activities: These refer to activities that place a significant burden on your metatarsal bones and joints, such as running, jumping, or dancing. Pressure over long periods will cause pain to increase, and some chronic pain will develop.
- Obesity: The simple physics of carrying extra weight results in more use with every step for your feet, causing more stress on the metatarsals. Otherwise, management symptoms are often weight reduction, a major modifiable factor given by the management.
- Medical conditions: Systemic conditions like rheumatoid arthritis or diabetes can cause inflammation in the feet or damage nerves over time, which causes metatarsalgia. It is crucial to manage these associated conditions appropriately.
- Foot injuries: Foot injuries, which result from moderate to severe overuse, can cause the metatarsals to become painful. The plan may usually be conservative, such as rest, ice, and good supportive shoes to offload the overstrained structures.
- Tight Achilles tendon and Morton’s neuroma: A tight Achilles tendon can alter a person’s gait mechanics, increasing stress on the forefoot. Morton’s neuroma is a tissue thickening in a nerve between the toes, where it can cause painful burning and a pebbly sensation, which can be confused with metatarsalgia.
- Prolonged standing on hard surfaces: For example, jobs that require prolonged standing on hard floors (i.e., in retail or a hospitality job), which may also exacerbate symptoms.
How is Metatarsalgia Diagnosed?
Metatarsalgia is diagnosed clinically by taking a proper medical history, performing a medical examination, and then obtaining imaging studies.
Physical Examination: The doctor will touch the foot and identify any areas of pain, as well as examine the general structure of your foot. They will also assess the mechanics of your walking (gait assessment) regarding weight transfer. Imaging will often be used to exclude other differential diagnoses and confirm the diagnosis.
Medical History: Some of the questions that a doctor might ask are “How much do you exercise?”, “What shoes do you usually wear?”, and “Where and what kind of pain is it in your foot that hurts?” Any other medical conditions, such as diabetes or arthritis, would be asked about. In the world of chronic pain, we say: document how it feels and what you do, the genesis of the pain, and its impact on your daily life.
Imaging Tests: Diagnostic imaging is an essential component of making the diagnosis because imaging can help exclude other diagnoses to better understand the source of your pain. The reason for this is that each imaging modality has a distinct purpose and offers a different perspective on the anatomy of the foot.
- X-rays: Bony structures of the foot are primarily evaluated using X-rays. A doctor usually orders an X-ray to determine if the lesions are stress fractures or deformities of the bone, like bunions or hammertoes, and to assess the alignment of the metatarsal bones. This tests if a structural problem is causing the metatarsalgia.
- Ultrasound: Involves the use of sound waves to produce images of tissues such as skin and systems within your body. This is useful for other types of problems besides bone issues, such as soft-tissue inflammation, bursitis, or a Morton’s neuroma (a thickened nerve). Neuroma is often diagnosed with an ultrasound, as it offers a real-time image.
- MRI: Magnetic Resonance Imaging, or MRI, is capable of producing a high level of detail for a variety of different body parts, from soft tissue structures to bone. When previous tests (like X-rays and ultrasounds) don’t show any problems or can’t determine the cause of your pain, a doctor may order an MRI, especially if they suspect a more complex issue like plantar plate injury or deep-seated inflammation. It provides the broadest look at the entire forefoot.
How is Metatarsalgia Treated?
Patients are treated with orthopedic foot supports in the first stage. Surgery is reserved for patients who have failed conservative measures or those with a severe deformity needing correction.
Non-Surgical Treatment
The cornerstone of conservative metatarsalgia care revolves around techniques to relieve the pressure on the sensitive metatarsal heads. This may include the use of supportive footwear, as well as other styles of inserts and padding. You should also avoid activities that are likely to cause excess force or strain the already aggravated tissues during the recovery period (while doing everything you can to facilitate tissue healing).
- Rest: Sit down and put your feet up. Take a break from doing the things that cause you pain. If pain persists, see a doctor.
- Ice: Use ice for 15–20 minutes a few times each day to help with swelling. Always wrap it in a towel.
- Pain Relievers: Get short-term relief of this pain with over-the-counter NSAIDs like ibuprofen, but bring in a doctor if you have other health conditions or are pregnant.
- Supportive Footwear: Choose footwear with a wide toe box, low heel, and cushioning. Replace running shoes. Runners should also look to replace their running shoes regularly -no high heels or thin soles.
- Orthotics/Inserts: The use of metatarsal pads and an arch support to take pressure off. This means that commercial insoles are entirely useless, and orthotics are an absolute must for these individuals to find relief.
- Cortisone Injections: For severe, unmanageable inflammation, some physicians may administer a cortisone shot. This can help reduce inflammation and eventually lead to relief.
Surgical Treatment
The surgical options are individualized to the underlying cause. Surgical procedures might involve bunion or hammertoe correction, bony realignment to rebalance pressure, or callus removal. Recovery usually includes some time in a cast and physical therapy. Although risks are minimal, they are present and should be discussed with the cosmetic surgeon.
- Correction of Deformities: Surgical correction may be necessary and often leads to a permanent solution for metatarsalgia since this issue is primarily driven by deformities such as bunions or hammertoes; with surgical realignment of the bones, pressure will also be more evenly distributed across the forefoot.
- Decompression Surgery: Decompression surgery is exceptionally uncommon and may be used as a last resort with failed treatment or when there is significant compromise of function. The goal of this procedure is to decompress the nerves or other structures in the forefoot. Recovery ranges can differ, and this is typically deemed the final alternative.
What are the Complications of Untreated Metatarsalgia?
Untreated metatarsalgia unlocks that door to the plethora of problems. Chronic pain can alter your gait, potentially causing new pain in your hips, knees, or lower back. Untreated, the pressure and inflammation may progress into a Morton’s neuroma (a thickened, painful mass of tissue often occurring on the ball of the foot), severe calluses that cause constant pain, or, more debilitatingly, slow-and-arrested but progressive toe deformities such as hammertoe.
Can Metatarsalgia Be Prevented?
Prevention consists of proactive protective measures with footwear, weight, and activity.
- Footwear: Wear shoes that have a wide toe box, a low heel, and great cushioning. For shoes with rocker soles, the goal is to redistribute the pressure. Change athletic shoes from time to time.
- Weight Management: Maintaining your healthy weight will ensure that pressure on your forefoot is minimized.
- Foot Exercises: Stretching the muscles of the foot, ankle, and Achilles tendons will help improve your foot mechanics and flexibility.
- Activity Modification: Change to less or non-weight-bearing activities, like swimming and stationary cycling, when having an exacerbation. Implement high-impact activities again gradually.
- Orthotics: These include orthotic products such as chewed-up metatarsal pad cushioning that cushions the ball of the foot with each step you make to prevent recurrence of the condition or improvement in such cases over mild to semi-rigid arch support.
- Callus Care: Treat calluses at home with a pumice stone to shave down the dead skin, but if they are thick and hard to remove, they should be shaved off in a medical setting by your doctor -this can help reduce pressure points-.
What are the Common Conditions that Cause Ball-of-the-Foot Pain?
Ball-of-the-foot pain, or metatarsalgia, represents a symptom and not a condition and may occur as a result of multiple conditions that have developed in the forefoot. These are the most typical contributors that should be understood to be diagnosed and treated effectively.
- Fat Pad Atrophy: Because of aging, the fat pad that cushions the bottom of your foot can be thinned, and pressure on the metatarsal bones can be increased. This particularly occurs among individuals who have diabetes.
- Capsulitis: Can cause bruise-like pain and swelling in the joint capsule at the base of a toe.
- Intermetatarsal Bursitis: It happens when the bursa, small fluid-filled sacs situated between the metatarsal bones, become inflamed, causing pain while weight-bearing.
- Plantar Plate Injury: If the ligament that stabilizes the toes is torn, pain may occur, and if left untreated, it can cause a toe to be deformed.
- Overuse: Pounding the ground with sports like running or jumping repeatedly can inflame the metatarsal heads and surrounding joints from overuse stress.
- High-Heeled Footwear: Putting on high heels causes your body weight to increase and puts pressure on the ball of your foot.
- Bunions (Hallux Valgus): Bunions are enlarged, bony bumps often at the base of the big toe, which in turn propels weight towards the lesser metatarsals.
- Hammer or Claw Toes: A deformity that causes toes to bend unnaturally around the metatarsal bones, causing excessive pressure.
- Claw Foot (Pes Cavus): A high arch distributes excess body weight more specifically through the ball of the foot and heel, necessitating an orthotic support built to fit exact contours.
- Morton’s Neuroma: Symptoms include thickening of nerve tissue between the third and fourth toes, causing a shooting, burning pain, and a sensation that you are walking on a pebble.
- Tight Achilles Tendon: A tight Achilles tendon will change your gait and increase the pressure on your metatarsals.
Moving Forward With Metatarsalgia Treatment
If you’re not feeling better after home treatment or if your pain is incessant and creating a change in the way you go about daily activities, it’s time to call in a professional. A professional diagnosis can get you the personalized treatment plan that you need, as well as custom orthotics or related equipment (which work much better than commercially available shoe inserts). Intervening early is essential to avoid the problem from becoming a chronic condition. That way, Dr. Jodi Schoenhaus, a metatarsalgia specialist, can provide the advanced care you require. Make an appointment today at the Foot, Ankle & Leg Vein Center to get back on your feet.
Metatarsalgia FAQs
Overloaded pressure and tension on the metatarsal bones in the forefoot are the primary cause of metatarsalgia. This may be as a result of several factors, such as high-impact exercises such as running, poorly supportive footwear (particularly high heels), orthopedic conditions such as bunions, and overweight status.
Yes, metatarsalgia usually clears up with conservative care like rest, ice, good shoes, and orthoses, but not always. If the root cause is not removed, over time, it may become a chronic problem.
No, metatarsalgia is by no means a form of plantar fasciitis. Even though the two often cause foot pain, they do so in different areas of the foot. Metatarsalgia describes pain and swelling of the ball of the foot (the forefoot), and plantar fasciitis is an inflammation of the plantar fascia, a piece of fascia that provides support to the ligaments of the foot across the bottom of the foot, connecting the heel to the toes.

